HCH 2022 Conference Session Materials
Pre-Conference Institutes | Tuesday, May 10
- Julia Dobbins, NHCHC
- Barbara DiPietro, NHCHC
- Leslie Enzian, Edward Thomas House Medical Respite
- Derrick Hoover, FAAFP Robert Wood Johnson Foundation Clinical Scholars Fellow
- Susannah King, Hennepin Health
- Brooks Ann McKinney, Cone Health and Hospitals/Triad Health Network ACO
- Pamela Mokler, Pamela Mokler & Associates, Inc.
- Annette Rodriguez, Yakima Neighborhood Health Services
Slides and other download materials:
Medical respite care bridges the gap between health care and housing continuum, offering people experiencing homelessness an opportunity to safely rest and recuperate from an acute medical need. Being situated between these two continuums can be challenging, but also provides significant opportunity for community partnerships.
This PCI will focus on how medical respite care programs can cultivate belonging among multiple community entities in order to meet the needs of their clients and disrupt the cycle of homelessness. Building effective program partnerships provides an opportunity not only for clients to address their health, but establish connections and belonging within their communities.
We will discuss strategies for building partnerships across your community, including with referring hospitals, behavioral health providers, managed care organizations/ health plans, and policy makers. This PCI will incorporate both didactic sessions and breakout discussions.
- Pamela Taylor, The Circle Works
Slides and other download materials:
The ongoing COVID-19 pandemic has caused high levels of burnout in the HCH community. High turnover, recruitment challenges, direct and vicarious trauma, and dramatic changes to health center operations have all contributed to staff feeling exhausted, overwhelmed, and chronically stressed.
A key strategy to mitigate the effects of this trauma is carefully facilitated discussions about it. With this goal, expert facilitators from The Circle Center will lead this full-day training that aims to equip participants with unique group facilitation skills that foster a deep and sustaining sense of connectedness and resilience during challenging times.
The Circle Process is rooted in the tradition of Talking Circles that Indigenous Peoples in North America use and have used for millennia. In this painful time in the movement to end homelessness, we invite community members to come for this unique opportunity both to learn how to cultivate collective resilience and to gain facilitation skills with the Circle Process to share with staff in their own health center. This session is recommended for all levels of health center staff, including administrative and clinical staff.
- Triza Laxmi Aurora, Valley Homeless Healthcare Program
- Lindsay Cross, Santa Clara Valley Medical Center
- Irene Guerra, Valley Homeless Healthcare Program
- Bridie Johnson, Colorado Coalition for the Homeless
- Baer Karrington, Seattle Children’s Hospital
- Alex Keuroghlian, The Fenway Institute
- Shawn Reilly, Vanderbilt University
- Paloma Sanchez, Colorado Coalition for the Homeless
- Shante Chunterry Lee Thomas, Valley Homeless Healthcare Program
Slides and other download materials:
Gender-affirming care is a life-saving intervention, especially for gender-diverse individuals experiencing homelessness. This full-day training is intended for participants interested in starting or expanding gender-affirming care services within their HCH programs. The training will include concurrent sessions for participants who are new to gender-affirming care and those who have provided gender-affirming care for years.
In partnership with Fenway Institute and other national experts, we will share foundational frameworks of gender diversity and how it intersects with homelessness. We will discuss best practices and innovative ideas around hormone therapy, developing community partnerships, gender-affirming surgery, behavioral health needs, and post-operative recovery.
Additionally, the group will engage in an interactive discussion on a constellation of intersecting issues including interpersonal violence, sex work, unsheltered homelessness, substance use, and mental wellbeing. Participants will have the opportunity to engage in information sharing and networking with clinicians from across the country.
Breakout Sessions | Wednesday, May 11
- Julia Lauryn Berner, NHCHC
- Katie League, NHCHC
- Caitlin Synovec, NHCHC
Slides and other download materials:
In the struggle to address homelessness with a lack of affordable housing, communities across the country have adopted and developed strategies to establish pathways to housing using prioritization. However, the past several years have demonstrated both the difficulty in prioritizing who is “most in need” of housing as well as inequities in the systems and tools utilized in this process.
In response to this realization, communities have identified a need to recreate and reimagine their processes to address inequities. Although no community has the “answer” to this challenge, several have identified promising models and lessons learned. This workshop will include a multi-disciplinary panel of individuals from across the country engaged in the process of building a more equitable system.
- Zenobia Smith, Boston Health Care for the Homeless Program
- Sonja M. Spears, Boston Health Care for the
- Morgan Ward, Boston Health Care for the Homeless Program
Slides and other download materials:
In the wake of nationwide calls for racial justice following the murder of George Floyd and the systemic racism and structural inequities laid bare by the COVID-19 pandemic, many organizations have vowed to strengthen their racial justice commitments and ensure that JEDI work keeps a seat at the table.
But does the space allotted shift in the presence of pandemic trauma, workforce challenges, and other competing considerations? What are some of the triumphs and challenges that arise when some fear this focus will reduce their elbow room or result in loss, as privilege and power shift while JEDI work is practiced and seems to be present for the long run? One HCH organization will share its experiences and lead an interactive discussion centered on the continued inclusion of JEDI work itself.
- Katy Bazylewicz, Cottage Health
- Monica Ray, Cottage Health
- Becky Santana, Cottage Health
Slides and other download materials:
Recuperative care plays a critical role in connecting the continuum of care for patients experiencing homelessness. For health systems, caring for patients and partnering on medical respite are both mission-aligned and integral to population health.
This workshop will share a model for health system-led respite, its development and implementation story, strengths to evaluation and funding, and how to partner with patients to increase equity. Health systems will learn the benefits of collaboration on recuperative care and its impact within the hospital and community. Shelters will gain insight to build relationships and strengthen communication with hospitals and patients. An open forum format will encourage participants to share their experiences with hospital and shelter collaborations.
- Tonya Bowers, Health Resources and Services Administration
- Richard S. Cho, U.S. Department of Housing and
Urban Development - Barbara DiPietro, NHCHC
- Emily Mosites, Centers for Disease Control and Prevention
- Jeff Olivet, U.S. Interagency Council on Homelessness
Slides and other download materials:
In this session, staff from various agencies will discuss priority issues, funding opportunities, and other issues pertinent to the HCH community. This session will provide a forum for open discussion about programs and issues vital to health center operations. Time will be reservedfor Q&A.
- Joseph Benson, Health Care for the Homeless Houston
- Katherine Cavanaugh, NHCHC
- Rodney Dawkins,
National Consumer Advocacy Board - Frances Isbell, Health Care for the Homeless Houston
Slides and other download materials:
In this session, staff from various agencies will discuss priority issues, funding opportunities, and other issues pertinent to the HCH community. This session will provide a forum for open discussion about programs and issues vital to health center operations. Time will be reservedfor Q&A.
- Jason Reinking, TRUST Clinic, LifeLong Medical Care
- Maria Zimmerman, TRUST Clinic, LifeLong Medical Care
Slides and other download materials:
Clinical outcomes for buprenorphine use in persons experiencing homeless (PEH) remain below national averages due to persistent barriers to care. Since 2017, depot (long-acting subcutaneous injection) buprenorphine has been an additional and formative pharmacological tool for use in opiate use disorders. However, its uptake and clinical application remain low.
Since 2019, our clinic has developed a robust depot buprenorphine program that has serviced more than 50 patients. In this presentation, we aim to build a case for the inclusion of depot buprenorphine in clinics serving PEH through exploration of our personal program data, program outcomes, and program operations while contextualizing our clinical experience through the firsthand sharing of patient narratives.
- Georgia Bright, Santa Clara University
- Caroline Cawley, University of California
- Jamie Chang, Santa Clara University
- Katherine Saxton, Santa Clara University
- Barry Zevin, Street Medicine and Shelter Health
Slides and other download materials:
- Ashley Meehan, Centers for Disease Control and Prevention
- Julia Rogers, University of Washington
Slides and other download materials:
- Casey Chappelle, Public Health, Seattle & King County
- Kami Harless, Public Health, Seattle & King County
- Julie Little, Public Health, Seattle & King County
Slides and other download materials:
On-demand services are critical to timely and patient-focused care of individuals experiencing homelessness. Our program provides low-barrier medical services by bringing our mobile teams directly to locations where individuals are sleeping or accessing other essential services. Our program provides a broad range of point of care testing, same-day procedures, and diagnostic/treatment services.
We strive to meet any medical/procedure/ diagnostic need that a patient may bring to our teams. This presentation will dive deeply into the overwhelming advantages of same-day services for individuals experiencing unstable housing while also laying the roadmap for all of the logistics, training, and preparation that goes into being prepared for anything that may walk up.
- Ken Kraybill, C4 Innovations
- Ann Marie Roepke, Evoke Training and Consulting, PLLC
Slides and other download materials:
Trauma-informed supervision is essential in settings where staff serve clients who are likely to have histories of trauma exposure and staff often experience secondary trauma exposure through their clinical work. In these extraordinarily challenging times in our world, trauma-informed supervision is more critical still. Whether you’re experienced, new, or not yet a supervisor, you are invited to learn more about applying a trauma-informed, healing-centered lens to supervision.
- Kyla Rankin, HOMES Program of Parkland Health and Hospital Systems
- Mollie Williams, The Family Van and Mobile Health Map
Slides and other download materials:
By literally meeting patients where they are, mobile clinics improve health outcomes and reduce health care costs. In our financially stressed health care systems, we must show funders, policymakers, and health care executives that mobile clinics make good business sense.
In this session, we will share a conceptual framework that describes how mobile clinics can bolster the business objectives of health care organizations, including those related to organizational culture, workforce capacity, health equity, and community partnerships. By aligning the goals of mobile programs with broader organizational strategies, health care leaders can make a strong case that mobile clinics are both good for community health and good for business.
- David Dirks, Homebase
- Mindy Mitchell, Homebase
Slides and other download materials:
This workshop, facilitated by experts in racial equity, coordinated entry (CE, and housing-health integration, will focus on strategies to utilize CE to identify and address racial and other inequities in access to housing, and ways HCH programs and other health stakeholders can participate in CE to ensure their clients – especially those who are Black, Indigenous, or other People of Color or who belong to other marginalized subpopulations – can access housing resources and other homeless assistance. Using a combination of community examples, Q&A, and group work, the workshop will have participants explore and define practical next steps to participate in and partner with CE systems to ensure equitable and efficient access to homeless system resources for particularly vulnerable clients.
- Irene Guerra, Valley Homeless Healthcare Program
- Jacqueline Newton, Valley Homeless Healthcare Program
Slides and other download materials:
Transgender, non-binary, and gender diverse (trans) people experiencing homelessness face discrimination and structural violence across their lifespans. A panel of trans consumers who have experienced homelessness will describe their unique healthcare needs.
The panelists will share how psychosocial trauma affects the sense of belonging and engagement in health care. Consumers will discuss how to adjust our approach to offer inclusive and equitable care. We will describe gender-affirming and trauma-informed approaches to street outreach, provider-patient communication, and clinical operations, and how to create spaces to build community. Panelists will discuss the impact of social isolation from clinic closure and telehealth, and how to adjust clinical practice during COVID-19.
- Rod Olin, Legacy Health
- Juliana Wallace, Central City Concern
Slides and other download materials:
In this workshop, we will review the existing clinical care models, best practices, challenges, opportunities, and data needed to compassionately address this crisis. The complex intersection of psychosis, violence, and treatment approaches demands us to engage in creative thinking, both in our development of care models and also in our policy and advocacy platforms.
- Rachel Biggs, Albuquerque Health Care for the Homeless
- Anita Cordova, Albuquerque Health Care for the Homeless
- Neil Greene, University of New Mexico
- David Modersbach, Alameda County Health Care for the Homeless Program
- Pia Valvassori, Health Care Center for the Homeless
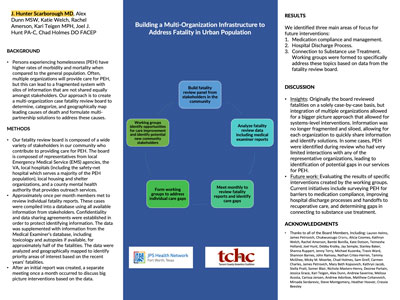
This workshop will help participants learn to start local mortality data reporting, drawing together experiences of three recently initiated regional/local homeless mortality report efforts. Presenters will draw on local efforts and participation in NHCHC’s Homeless Mortality Data Work Group.
Specific examples, processes, and tools will be shared to help beginners start a mortality count in their cities, and the local conditions to draw on to start homeless mortality reporting: local health departments; medical examiners/coroners; homeless data matching; and community partners. Discussion will focus on increasing data collection, how to interpret mortality data and use it to drive local change, and how we can improve and standardize homeless mortality data to drive policies and practice.
- Moffett Burgess, Public Health Seattle & King County
- Deborah DeQuier-Bowden, Public Health Seattle & King County
- Aji Jobe, Public Health Seattle & King County
Slides and other download materials:
Equitable Health Practices in the Provision of Dental Care for People Experiencing Homelessness: A significant health equity issue people experiencing homelessness are confronted with is oral health. Toothaches, dental abscesses, and tooth loss show disparities in prevalence. These problems challenge people’s well-being and can interfere with all aspects of life, including belonging and dignity.
The added stresses of limited access to care, financial barriers, and fear of treatment complicate dental care in ways that differ from other disciplines. We provide examples of patient-centered practices we implemented to cut through barriers to wellness. We focus on examples of how clinical teams use principles of inclusion and belonging to support good health outcomes.
- Anthony Coleman, Housing for Health
- Ruby Romero, University of California, Los Angeles
Slides and other download materials:
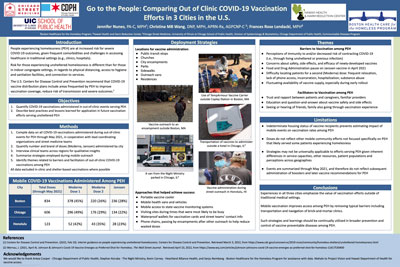
Through a partnership between two organizations, the Peer Ambassador (PA) Program was implemented to help increase vaccination against COVID-19 among sheltered and unsheltered people experiencing homelessness (PEH).
During this workshop, the focus will be on COVID-19 vaccination efforts in the unsheltered setting. The aim of this workshop is to educate others on the role of PAs, share what has been found to be the best practices for implementing the program, and encourage attendees to implement similar programs.
- Cheryl Ho, Valley Homeless Healthcare Program
- David Meyers, Valley Homeless Healthcare Program
- India Rogers-Sharp, Stanford School of Medicine
- Paul Williams, Valley Homeless Healthcare Program
Slides and other download materials:
In this session, participants will learn about the current state of the literature with regard to medical outcomes in permanent supportive housing (PSH). Different models of housing support from other HCH programs across the country will be reviewed. Early results (quality of life, social isolation, mental health, and substance use) from one program’s two-year study will be summarized.
In addition, participants will have an opportunity to hear common themes and voices from a set of qualitative interviews and a current PSH program consumer. In the last part of the workshop, participants will dialogue together as a group to propose ideas for more consumer-centered, trauma-informed models for future permanent supportive housing.
- Kami Harless, Public Health Department of Seattle & King County
- Amy Kennedy, University of Washington School of Medicine/VA Puget Sound Healthcare System
- Lisa Herrera Perales, Public Health Department of Seattle & King County
Slides and other download materials:
In the United States, there are approximately 1.2 million people aged 13 and older living with HIV, and an estimated 34,800 new HIV infections every year. Despite major advances in the prevention of HIV, our most marginalized neighbors continue to see a disproportionate risk of acquiring HIV. Providers caring for patients experiencing homelessness play a central role in taking care of people who are at higher risk for HIV infections.
Initiating HIV pre-exposure prophylaxis (PrEP) and antiretroviral therapy (ART) in a timely manner improves patient outcomes. We will provide a model for low-barrier access by providing point-of-care HIV testing and same-day initiation of PrEP or ART. This lecture will be a case-based session with didactic interspersed with clinical cases and polling questions, and will focus on HIV screening, prevention, diagnosis, and rapid start of ART.
- Charissa Fotinos, Washington State Health Care Authority
- Barbara DiPietro, National Health Care for the Homeless Council
- Rhonda Hauff, Yakima Neighborhood Health Services
- Kat Ferguson-Mahan Latet, Community Health Plan of Washington
- Sheela Tallman, UnitedHealth Group
Slides and other download materials:
Medicaid reimbursements for medical respite care are a key strategy for program stability and improved client outcomes. As states consider how to move forward with financing these models of care, one state’s process may serve as a template for others to replicate.
This panel discussion will cover the advocacy, policy issues, and stakeholder engagement needed for successful statewide planning, and will build off a recently published state legislative report. Come to this conversation to hear from Medicaid officials and HCH-medical respite care leaders, and talk about what is working best in states to move forward to adopting medical respite at a systems level of care.
- Matt Bennett, Optimal Innovation Group
Slides and other download materials:
The challenge that faces us is clear: How do we help a burned-out and traumatized workforce recover? We cannot assume this healing will naturally happen as vaccines help us return to “normal.” If not strategically addressed, our workforce’s mental health threatens to lower our outcomes, devastate our organizational culture, and cost us financially in turnover, absenteeism, health care costs, and declining productivity.
This workshop will help leaders and managers understand the impact of the trauma of the last months, create a recovery plan, and address the systematic issues that burned people out at alarming rates before the pandemic.
- Terri Cooley-Bennett, Swope Health Services
Slides and other download materials:
Suicide rates have increased rapidly in the nation and individuals experiencing homelessness are at great risk for suicidality. Risk factors are high among the homeless population, including unemployment, early adverse childhood experiences (ACES, substance use, chronic health conditions, mental health problems, and a lack of support, among others.
It is critical for professionals in Health Care for the Homeless programs to understand suicidality and to be well-informed regarding suicidality and suicide prevention. Licensing boards require regular suicide prevention training. This workshop will discuss the prevalence of suicidality among homeless populations, including sub-populations. Best practices, treatment methodologies, and resources to address vicarious trauma will be discussed.
- Bridie Johnson, Colorado Coalition for the Homeless
Slides and other download materials:
This presentation goes into a deeper understanding of the Two-Spirit identity and how the indigenous population has lost its way in regard to supporting LBGTQIA individuals in their own tribes and/or urban settings and communities they live in currently.
We will explore Indigenous historical trauma and how impactful Christianization, Catholicism, and Colonization were on their identity formulation. Pre-colonization, they were revered as heroes in the indigenous communities in which they were reared.
- Amy Grassette, Family Health Center of Worcester
- Stefan Kertesz, University of Alabama, Birmingham
- Megan Leubner, Frank H. Netter MD School of Medicine at Quinnipiac University
- James O’Connell, Boston Health Care for the Homeless Program
Slides and other download materials:
- Dan Bergholz, Miami Street Medicine
- Brett Feldman, KSOM of USC Street Medicine
- Corinne Feldman, KSOM of USC Street Medicine
- Armen Henderson, University of Miami Medical School
- Sabrina Hennecke, Miami Street Medicine
- David Peery, Camilus Health Concern
Slides and other download materials:
Part 1: We will begin with a facilitated discussion of how PEH are currently utilized as educators. Next, we will highlight a one-year experiential learning opportunity where an interdisciplinary team of students are guided through the system by a current street medicine patient experiencing difficulty accessing health care and social services. Program design specifics, including student/patient selection and curriculum, will be discussed.
Part 2: We then will discuss how an innovative Advocacy Unit has been implemented by Miami Street Medicine (MSM), in which medical students and physicians have monitored and brought examples of this patient harm to local media.
This advocacy mobilized advocates and resulted in a large protest of the city’s effort to ban homeless encampments. This success suggests a model strategy of using street medicine advocacy to formulate compelling narratives against homelessness criminalization, which can be replicated nationwide.
- Carrie Craig, Colorado Coalition for the Homeless
- Catherine Crosland, Unity Health Care
- Lawanda Williams, Baltimore Health Care for the Homeless
Slides and other download materials:
It is undeniable that a significant portion of populations experiencing street homelessness suffer from severe mental illness. We would like to facilitate an open and honest conversation about the topic of involuntary treatment of mental illness in this country.
We will use a moral decision-making framework and bring in perspectives from other countries in which the perspective differs slightly toward a “right to appropriate treatment of mental illness” versus the perspective widely held in the U.S. of “the right to self-determination.”
- Lina Barbenes, Montefiore Hospital
- Carolina Miranda, Montefiore Hospital
- Ian Zdanowicz, Queer Detainee Empowerment Project
Slides and other download materials:
This workshop will present an innovative care delivery model serving one of the most marginalized populations of our time: houseless transgender and non-binary (TGNB immigrants who have been detained while being involved in immigration proceedings, including asylum. Using an interdisciplinary approach, our partnership between a Federally Qualified Health Center and an LGBTQIA community-based organization provides affirming, inclusive, and culturally humble mental health, medical, and sociopolitical care.
Because the TGNB asylum-seeking community experiences the compounded traumas of social isolation, persecution, migration, and immigration detention, a community-based approach is uniquely suited to meet our patients’ need for support and a sense of belonging.
- Anthony Coleman, Housing for Health
- Chelsea L. Shover, University of California, Los Angeles
- Joanna Swan, Housing for Health
- Sieglinde Von Deffner, Housing for Health
Slides and other download materials:
The first part of this workshop will present a case study of how government, academic, and community partners worked together to dramatically scale up naloxone distribution to people experiencing homelessness.
The four presenters — a licensed clinical social worker, a public health researcher, and two community health workers — can speak to different dimensions of the effort, from incorporating harm reduction into other health outreach, to state-level policy change to get 100,000 doses, to reversing overdoses using the additional kits. The second part will be a group exercise with three steps: a describe a problem in their jurisdiction that might be helped with a policy action; b identify policy levers; and c network to find potential partnerships.
- Jacqueline Cameron, Cook County Health
- Kristen Dickins, Massachusetts General Hospital
- Keiki Hinami, Cook County Health
- Miao Jenny Hua, Cook County Health
Slides and other download materials:
In 2021, the National Health Care for the Homeless Council published its Homeless Mortality Tool Kit in support of jurisdictions seeking to apply data toward informed resource allocations and advocacy. In this presentation, we introduce distinct use cases of such data from Boston and Chicago.
- Fiona Asigbee, Cottage Health
- Anna Pruitt, University of Hawai’i , Manoa
- Landon Ranck, Santa Barbara Alliance for Community Transformation
Slides and other download materials:
This workshop will discuss the potential of community-based participatory research (CBPR) methods for understanding lived experiences with homelessness and creating trust and belonging. Based on a Photovoice study examining how the COVID-19 pandemic is impacting people experiencing homelessness in a California county, lessons learned from engaging in CBPR during a pandemic will be discussed.
Researchers will share strategies for collecting data from a variety of homelessness communities (e.g., unsheltered, sheltered, and vehicular) and will explore best practices for engaging multiple community partners and building trust within the homelessness community. Using a photo wall and lived experiences of co-researchers, this workshop will demonstrate how CBPR can empower homeless communities.
- Rachel Biggs, Albuquerque Health Care for the Homeless
- Nadia Fazel, Albuquerque Health Care for the Homeless
- Jennifer Metzler, Albuquerque Health Care for the Homeless
This workshop will engage participants in learning how to leverage the community of HCHs to collaboratively engage shelter provider partners, health care systems, and public health departments in effective policy change during public health emergencies.
HCHs emerged as essential partners during the COVID response that bridged the gap between homeless assistance providers and public health entities. This workshop will walk participants through the process of amplifying the work of HCHs across the country to inform a local response to COVID for people without homes. Presenters will share lessons learned on how to bring together clinical, public health, and policy staff to position the organization as central to a coordinated response and management system.
- Scott Ikeda, Bronx Health Collective, Montefiore Medical Center
- Mariel Lougee, Contra Costa Healthcare for the Homeless
- Alan Shapiro, Montifiore Medical Center
- Misty Webb, CORE Outreach
Slides and other download materials:
Poster Presentations | Wednesday, May 11
Breakout Sessions | Thursday, May 12
- Jennifer Battis, C4 Innovations
- Kellyann Day, New Reach, Inc.
- Beth Klink, Yale-New Haven Hospital
Slides and other download materials:
A leading agency in providing housing and supportive services, along with a local hospital and external evaluator, will discuss an evaluation and quality improvement project that is effectively helping cisgender and transgender women who are experiencing homelessness, have co-occurring disorders, and are high hospital utilizes.
The presentation will focus on the high-quality data and metrics methodology and how it has informed and transformed the partnership’s work and success in helping the targeted marginalized subpopulation to attain equitable and high-quality trauma-informed care. The presentation will focus on the challenges faced by the intensity of cases, and how the partnership and data-informed processes are positively affecting the health and housing of these women.
- Jennifer Hartley, Fora Health
- Eowyn Rieke, Fora Health
Slides and other download materials:
The presence of fentanyl and fentanyl analogues (F/FA in the U.S. drug supply has contributed to dramatic increases in overdose deaths, as well as new challenges in Medications for Opioid Use Disorder (MOUD care. Inductions for patients using fentanyl present a higher risk of precipitated withdrawal as well as other complex reactions.
Patients may give up on MOUD after an unsuccessful induction. These same difficulties may lead medical providers to limit the patients to whom they offer buprenorphine because of difficult experiences with inductions. Low-dose induction is a viable alternative, though patients and withdrawal management programs often struggle with the length or complexity of this process.
- Victor Cruz, King County Public Health
- Eric Skyler Jones, King County Public Health
- Martin Reinsel, Reinsel Consulting
Slides and other download materials:
This workshop focuses on the emerging “staff support” needs evident during the advancement of COVID-19. The burdens on staff striving to provide quality care during a pandemic were clearly evident to organizational leaders in 2020. Signs of burnout emerged.
The primary impacts of COVID-19 affected some staff members’ (and their loved ones’ health. An abundance of secondary concerns emerged as well, professionally and personally. Staff experienced secondary trauma at work: witnessing increased suffering, losing contact with patients during the pandemic, and being unable to provide the usual quality of care and/or providing care amidst additional strain (e.g, working outdoors in tents. This presentation focuses on the contract services providing “trauma-informed staff support” to assist staff.
- Miguel Ibara, San Francisco Community Health Center
Slides and other download materials:
Project REACT is a community-based, multi-partner, multidisciplinary, culturally appropriate, and highly tailored service focused on supporting populations and neighborhoods most disproportionately impacted by COVID-19 in San Francisco.
In action, Project REACT provides: targeted prevention and risk-reduction outreach and health education on COVID-19, HIV, Hep-C, and other STIs; promotion of COVID-19 testing and vaccines; mobile testing and vaccine support targeting consumers experiencing hesitancy; and much more. During this presentation, attendees will have an opportunity to learn about Project REACT, the creation of a unified response to COVID-19 and other epidemics impacting consumers, and tools to implement their own field-based health engagement and Community Ambassador programs.
- Marie Black, MBI Health Services, LLC
- Catherine Crosland, Unity Health Care
- Dan Hasan, Department of Human Services
Slides and other download materials:
The COVID-19 pandemic crystallizes how homelessness is a public health crisis and that housing is health care. Isolation and quarantine guidelines prescribed by the CDC and local health departments do not work for people experiencing homelessness who often live in congregate shelters and encampments.
Against this backdrop, our HCH and the local Department of Human Services partnered to create a three-pronged emergency response for people experiencing homelessness that includes the reactive strategy of creating isolation and quarantine hotels, the proactive strategy of creating protective hotel shelters for older and medically vulnerable individuals and a comprehensive testing and vaccination strategy. This session describes this collaboration, best practices, and lessons for the future.
- Edward Adair, Hennepin Healthcare Research Institute
- Moncies Franco, Hennepin Healthcare Research Institute
- Amy Kennedy, University of Washington School of Medicine/VA Puget Sound Healthcare System
- Denita Ngwu, Hennepin Healthcare Research Institute/Hennepein County Health Care for the Homeless
- Katherine Vickery, Hennepin Healthcare Research Institute/Hennepein County Health Care for the Homeless
Slides and other download materials:
- Diana Aycinena, San Francisco Community Health Center
- Shannon Heuklom, San Francisco Community Health Center
Slides and other download materials:
Rapid deployment of vaccines is essential to control the COVID pandemic. The Tenderloin community in San Francisco has many barriers to vaccination, including non-participation in traditional health care, health care mistrust, homelessness, inability to take time off of work, and active substance use.
A program was developed with several local organizations to create a stationary vaccine clinic. It was realized that traveling even several blocks was a sufficient barrier to deter people from getting vaccinated. A rapid intervention was developed that brought healthcare providers and vaccines directly to people rather than trying to get people to the vaccine site.
- Katherine Cavanaugh, NHCHC
- Kendall Clark, Mary Eliza Health Center
- Charlotte Garner, Health Care for the Homeless Houston
- Deidre Young, Health Care for the Homeless Houston
Slides and other download materials:
- Frances Driscoll, Baltimore Health Care for the Homeless
- Deirdre Hoey, Baltimore Health Care for the Homeless
- Albert Miller, Baltimore Health Care for the Homeless
Slides and other download materials:
Using the principles of polyvagal theory, this workshop will provide education about the nervous system and demonstrate how an accessible, inclusive, trauma-informed style of yoga practice can improve health outcomes and build a stronger community.
Experiences of homelessness can overload the body with trauma response symptoms (such as numbness, cognitive problems, impulsive behaviors, and isolation. Difficulty maintaining trust and seeing the world as unsafe can inhibit consumer, provider, and peer relationships. The drive to survive is at odds with a longing for connection. Yoga is one way to help access feelings of calm and unity in the midst of homelessness.
- Julia Dobbins, NHCHC
- Caitlin Synovec, NHCHC
Slides and other download materials:
Medical respite care provides a safe place for healing and recovery from acute health care events for people experiencing homelessness. Within these programs, providing trauma-informed care is essential. A critical element of trauma-informed care is providing a safe and healing environment; one that is accessible, comforting, and promotes recovery.
This session will provide an overview on creating a healing environment within your medical respite program. This session will be applicable to developing and established programs, with a large or small budget, and for a variety of clients served.
- Katie Burk, Facente Consulting
- Brenda Cantero, National Harm Reduction Coalition
- Porsha Dixson, National Harm Reduction Coalition
- Laura Guzman, National Harm Reduction Coalition
- Kristen Marshall, National Harm Reduction Coalition
Slides and other download materials:
Compared to non-single room occupancy hotel (SRO) residents, residents of SRO hotels are 19 times more likely to die of an accidental overdose death. The program works with staff and residents of supportive housing SRO hotels to ensure a community-led approach to overdose prevention efforts.
Attendees of this workshop will learn about the program components and the structural and institutional barriers program staff confronted during program implementation, including COVID-19 restrictions and impacts. Workshop attendees will participate in a facilitated discussion around the vulnerability of SRO residents, addressing barriers to program implementation, and strategies to involve supportive housing staff and residents in overdose prevention.
- Shatrice Grimes, Country Doctor Community Health Centers
- Laura Morgan, Country Doctors Community Health Centers
- Anna Steiner, Transitions Clinic Network
Slides and other download materials:
Transitions Clinic Network (TCN) supports a national network of medical homes dedicated to serving people returning from incarceration. TCN programs are implemented in primary care clinics located in communities impacted by incarceration and integrate community health workers with lived experience of incarceration onto primary care teams.
In this workshop, TCN will provide an overview of the systemic barriers to continuity of care for people leaving incarceration, how incarceration impacts health, and ways that community health systems can mitigate the lasting harms of mass incarceration. Staff from Country Doctor Community Clinic (Seattle) will introduce their TCN program and explain how and why health systems serving people experiencing homelessness are primed to implement this program.
- Ed Farrell, Colorado Coalition for the Homeless
- Tom Gray, Denver Health
- Myra Nagy, Denver Health Project HOPE
- Laura Podewils, Denver Health
- Leah Shaw, Boston Health Care for the Homeless Program
- Sarah Stella, Denver Health; University of Colorado School of Medicine
Slides and other download materials:
- Jadie Hokuala Iijima Geil, Hui Aloha
- Linday Ann Pacheco, Ka Po’e O Kaka’ako/Hui Aloha
- Claudia Powell, University of Arizona Southwest Institute for Research on Women
- Anna Pruitt, University of Hawai’i at Manoa
Slides and other download materials:
- Ed Farrell, Colorado Coalition for the Homeless
- Ken Kraybill, C4 Innovations
- Ann Marie Roepke, Evoke Training and Consulting
Slides and other download materials:
While tending to people’s needs in the moment, you also hope they’ll make specific changes to improve their health and well-being. But your time is limited. You’re already trying to squeeze in a lot during each encounter. And perhaps your previous attempts to “get” them to change have been less than effective.
The good news is that there are some brief, simple strategies to increase the likelihood of people making positive changes. In this workshop, you’ll be invited to observe and “try-out” some ways to engage people in conversations about change, help them determine change goals, evoke their own hopes and ideas supporting change, develop an achievable plan, and provide information and advice in a guiding style. Practitioners of all disciplines are welcome.
- Lawrence Chang, Valley Homeless Healthcare Program
- Sophie Nguyen, Valley Homeless Healthcare Program
- Michael Wong, Valley Homeless Healthcare Program
Slides and other download materials:
Utilizing their specialized knowledge in medications, guideline-recommended treatments, and navigating insurances/formularies, clinical pharmacists are equipped to make significant clinical impacts when managing chronic disease states in an interdisciplinary team within a primary care clinic, as proven by a multitude of published studies throughout the country.
This session will aim to describe the role, methods, and benefits of clinical pharmacists operating in an FQHC primary care clinic by specifically tracking health outcomes in homeless patients seen in 2021 and outlining innovative practices shown to be effective for homeless patients. Outcomes that will be presented include blood pressure, A1c data, hepatitis C treatment outcomes, medication adherence, and hospital readmission data.
Slides and other download materials:
This is a listening session for Clinicians of Color and is an opportunity to assist Council staff in identifying upstream inequities including, but not limited to, institutional inequities, social, and political determinants of health that impact one’s health and the ability to perform at one’s workplace.
Questions will be posed to the attendees with short discussions on various topics. Our definition of clinicians is very broad and welcome all health center staff to this session.
- Rodrigo Avila, University of California, San Francisco
- John Friend, University of California, San Francisco
- Janet Grochowski, University of California, San Francisco
- Elizabeth Lynch, University of California, San Francisco
Slides and other download materials:
The traditional model of primary care creates significant barriers for unstably housed communities to access patient-centered care including rigid appointment schedules and lack of onsite behavioral health services. An HIV primary care clinic located in a dense urban setting has operationalized a drop-in care program that caters to the specific needs of PEH.
Despite challenges, the core of this program’s success has been consistent team communication, non-hierarchical interdisciplinary collaboration, and a focus on relationship-based care. This workshop will describe core elements of this successful longitudinal care model: data-driven care management e-dashboard, interdisciplinary conference formats, and panel management strategies. Attendees will be able to apply lessons learned to their clinics.
- Thomas D. Huggett, Lawndale Christian Health Center
- Mary Kate Schroeter, Chicago Department of Public Health;
- Mary Tornabene, Heartland Alliance Health
Slides and other download materials:
The impact of COVID-19 on sheltered communities brought about new collaborations and innovative systems of shelter-based care delivery. This interactive multimedia presentation will detail how the health authority and two FQHCs came together, guided by the shared value of equity, to serve our participants.
We will discuss our successes and challenges, creative use of COVID-19 funding and contracting, mutually agreed upon scopes of service, standards of care, outcomes of shield and supportive housing, and vaccine efforts. We will outline our efforts to meet our overarching goal that each sheltered person in the city has one visit with an HCH expert.
- John Barlie, University of Hawai’i, Manoa
- Amy Fairweather, Swords to Plowshares
- Pauline Lubens, Swords to Plowshares
- Monet Meyer, University of Hawai’i, Manoa
- Anna Pruitt, University of Hawai’i, Manoa
Slides and other download materials:
- Mercy Egbujor, Valley Homeless Healthcare Program
- Dirk Everett, Valley Homeless Healthcare Program
Slides and other download materials:
- Kelly Campbell, Harborview Medical Center
- Joseph Hulford, Harborview Medical Center
- Ian Johnson, University of Washington
- Michael Light, Harborview Medical Center
Slides and other download materials:
The Healthcare for the Homeless Palliative Care Team is the first mobile outreach palliative care program in the United States serving people experiencing homelessness or living in supportive housing.
This presentation by program staff and our research partner describes issues impacting unhoused patients when facing serious illness or end-of-life. They describe their novel program model, including roles in clinical care, collaborative care management, consultation, and community education.
They also present findings from a mixed-method retrospective chart review of program participants highlighting factors determining locations of care, facilitators for care in shelters and encampments, and barriers to equitable system interventions.
- Katie Kuehl, Washington State University College of Veterinary Medicine
- Vickie Ramirez, University of Washington – Center for One Health Research
- Anina Terry, Neighborcare Health
Slides and other download materials:
This workshop will present an innovative model of health care providing integrated veterinary and human health care to youth and young adults experiencing homelessness and housing insecurity with pets.
The purpose of this interdisciplinary, holistic approach is to reduce barriers to accessing care and to increase engagement in primary and preventative health care for both the human owner and pet. Data collected since model implementation in 2018 at a small FQHC satellite clinic shows a 42% increase in new patients engaging in health care and an 18% increase in follow-up human health care.
A free online toolkit, created by the team that established this care model in collaboration with a community advisory board, will be presented as a resource for model implementation in other care settings.
- Carrie Craig, Colorado Coalition for the Homeless
- Lisa Thompson, Colorado Coalition for the Homeless
Slides and other download materials:
The Denver Social Impact Bond was a five-year program to house 250 chronically homeless individuals who had frequent interactions with the criminal justice system in order to create housing stability and achieve a reduction in jail-bed days for program participants and achieve cost savings for the City of Denver.
To accomplish these goals, a strong public-private partnership was built to design and implement the program and to track, evaluate, and report out on the results. The results were very positive for people experiencing chronic homelessness and the community as detailed in the final report released in July 2021.
- Miriah Nunnaley, Colorado Coalition for the Homeless
- Sossity Perkins, Colorado Coalition for the Homeless
- Pia Vavassori, Health Care for the Homeless, Orlando
- Stephen Wilder, NHCHC
Slides and other download materials:
Medical respite care (MRC) remains widely under-researched, and the perspectives of people with lived experience of homelessness (PLE are under-represented in the existing literature. In response to this dearth of research, a year-long, PCORI-funded stakeholder engagement project was implemented to identify research priorities for MRC and ensure that the voices of PLE are at the center of future research efforts.
This workshop will highlight the project’s robust findings and will serve to educate participants about research objectives in MRC, equip them with engagement strategies tailored to the needs of PLE, and collaboratively explore opportunities to plan, implement, and disseminate inclusive and participatory research that demonstrates the impact and value of MRC.
- Julie Little, King County Public Health
- Kammi Lopez, King County Public Health
- Carrie Reinhart, King County Public Health
- Penelope Toland, King County Public Health
Slides and other download materials:
This workshop presentation highlights the challenges, outcomes, and importance of providing trauma-informed and accessible STI screening and treatment to people living unsheltered. The team will present their testing and treatment data and complex case studies. In comparison to clinic-based treatment, field-based treatment allows for more flexibility and adaptation to a client’s needs, leading to patient-centered and low-barrier care.
By offering harm reduction and basic needs supplies first, the patient’s goals are at the center of all medical visits. By truly meeting people where they are, offering point-of-care testing, and administering medications for treatment in the field, the outreach team has developed a system to better serve the sexual health needs of unhoused individuals.
- Albert Parramon, Central City Concern
- Juliana Wallace, Central City Concern
Slides and other download materials:
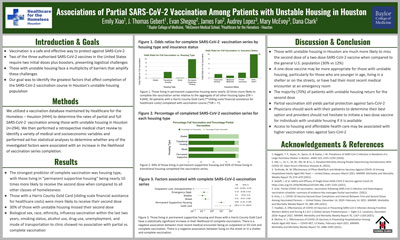
- Katherine Benandi, UT Houston School of Public Health
- Anna Jackson, Gateway Community Service Board
- Ben King, University of Houston
- Sitwat Malik, Gateway Community Service Board
- Victoria Warren, University of Houston
Slides and other download materials:
Learning Labs | Friday, May 13
- Lisa James, Futures Without Violence
- Surabhi Kukke, Futures Without Violence
- Rebecca Levenson, Futures Without Violence
- Anna Marjavi, Futures Without Violence
- Sarah Scott, Futures Without Violence
- Camila Sanchez Tejada, Futures Without Violence
Slides and other download materials:
In partnership with Health Partners on IPV + Exploitation, the Council is excited to offer this half-day training intended to equip participants with skills to support survivors of interpersonal violence (IPV experiencing homelessness through community partnerships and healing-centered engagement strategies. Participants will learn how to build MOUs and similar agreements with their local IPV agencies and how to have conversations about healthy relationships with patients/consumers.
Slides and other download materials:
Ensuring the safety of patients and staff without compromising trauma-informed care can be a challenge. Join the National Consumer Advisory Board as we discuss and discover together trauma-informed, patient-approved methods for creating a safe patient experience and for addressing threats and challenges to security within the health center and in outreach.
- Jen Elder, SAMHSA Homeless and Housing Resource Center
- Cheryl Ho, Valley Homeless Healthcare Program
- Lauren Velez, Corporation for Supportive Housing
- Paul Williams, Valley Homeless Healthcare Program
Slides and other download materials:
The transition from homelessness to housing can involve complex processes of navigating new services, neighborhoods, relationships, and housing rules. This transition can be difficult, particularly for individuals living with behavioral health conditions, and there are risks of worsening mental health status, overdose, and losing the new tenancy.
This Learning Lab, led by SAMHSA’s Homeless and Housing Resource Center, will explore best practices for supporting transitions to housing for individuals living with behavioral health conditions. Participants will discuss strategies for strengthening community partnerships, creating person-centered transition plans, and trauma-informed practices that help new tenants succeed in housing.
Slides and other download materials:
We will learn from experts across the HCH community about best practices and emerging strategies in the management of chronic illness among people experiencing homelessness. Focusing on diabetes and COPD, we will explore approaches for team-based care and supporting clients’ self-management, and discuss quality improvement strategies. Join us and come prepared to share ideas and learn from each other.
- Kevonya Elzia, Neighborcare Health
Slides and other download materials:
“Intersectionality is a lens through which you can see where power comes and collides, where it interlocks and intersects. It’s not simply that there’s a race problem, gender problem, class problem, or LBGTQ problem.
Intersectionality can get used as a blanket term to mean, “Well, it’s complicated.” Sometimes, “It’s complicated” is an excuse to not do anything. We want to move beyond that idea. We aim to do a deep dive into anti-racism as both individuals and as Health Care for the Homeless organizations breaking through the many challenging layers confronting our patients and ourselves.
In this two-part workshop, we will demonstrate the role of intersectionality and a healing-centered approach in moving HCH organizations and staff toward embodying anti-racism at the institutional level.
IN MEMORIAM: This Learning Lab is dedicated to Marcia Tanur, physician at Harbor Care, who passed away unexpectedly in February. She was also the medical director for the Methamphetamine Treatment Program. Marcia was slated to be a co-presenter and her work contributed significantly to this Learning Lab.