By Barbara DiPietro, PhD, Senior Director of Policy
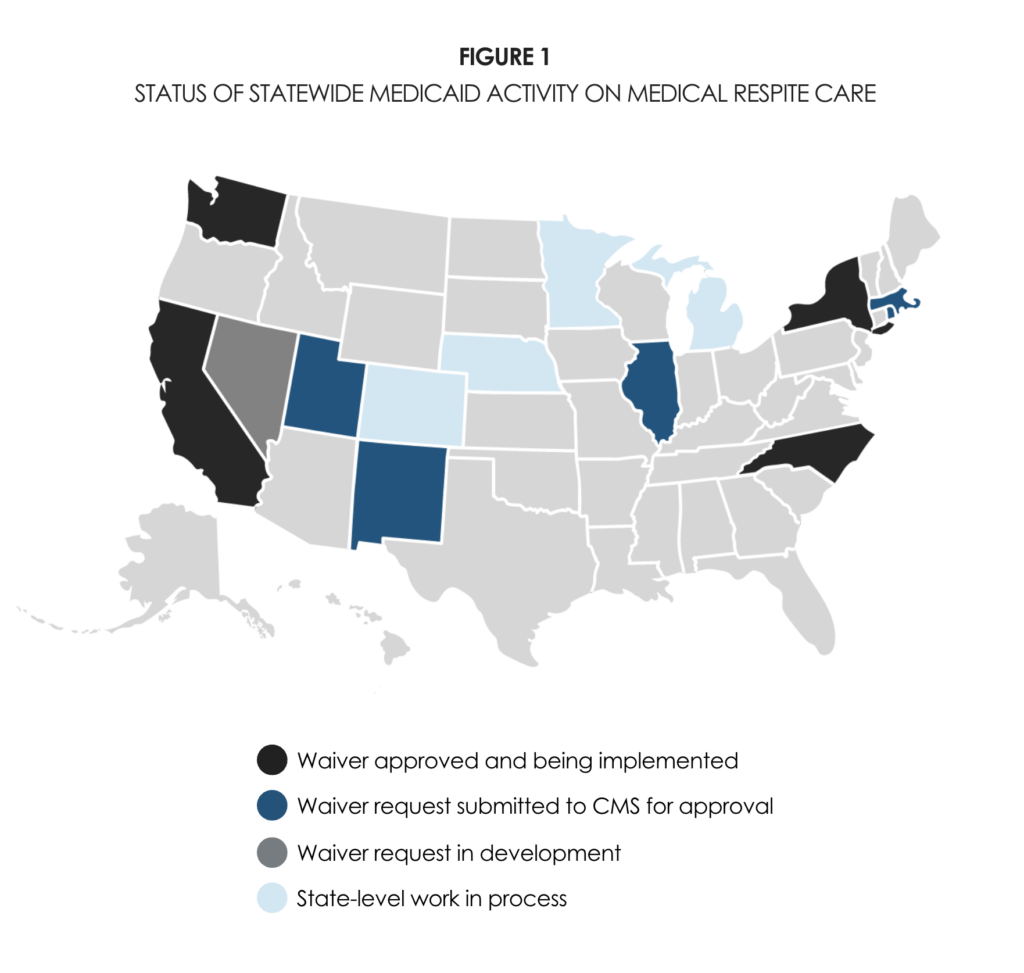
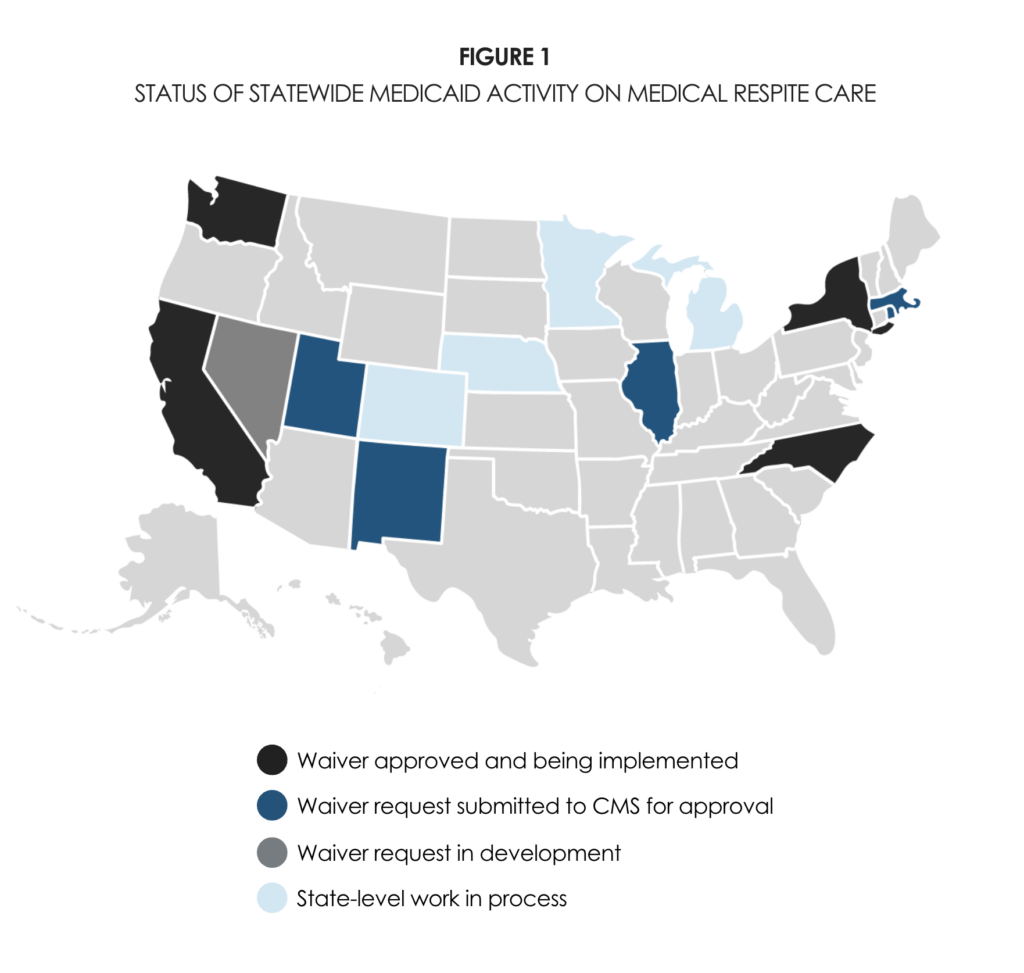
I’m excited to share two new issue briefs that focus on the role of Medicaid in paying for medical respite care. Our first brief — Status of State-Level Medicaid Benefits for Medical Respite Care — provides a current snapshot of the state-level Medicaid activity related to medical respite care. The map in Figure 1 below shows the 14 states already paying for medical respite care through Medicaid — or actively getting ready to do so.
This is incredible progress for a field that has been operating for nearly 30 years yet has not been fully recognized by many health care stakeholders. Since 2014, the expansion of Medicaid to single adults in most states, the growing recognition of the impact of social determinants of health, and federal policy that allows Medicaid to cover a wider range of services have broadened the funding for new approaches to care. The medical respite community — led by the fiercely dedicated Respite Care Providers’ Network and the Council’s rapidly growing medical respite team — has put in the time, advocacy, and research needed to make financial sustainability a greater reality. We are rapidly moving to make medical respite care part of the mainstream health care system — and funded accordingly.
California was the first to adopt Medicaid for recuperative care* as a statewide service. Our second brief — CalAIM Implementation of Recuperative Care Services: Lessons Learned — documents what is working well with the implementation of the CalAIM recuperative care service to date, what remains a challenge, action steps California should consider moving forward, and advice for other states looking to add a statewide Medicaid benefit for recuperative care. With New York, North Carolina, and Washington also in implementation stage (and others close behind), this is a good time to learn from others’ experiences and advocate for strategies that make for easier transitions to statewide reimbursement.
However: Being part of the mainstream health care system in the U.S. comes with a significant downside. One of the key takeaways from the California brief is that billing insurance is a sizeable administrative burden, especially for smaller programs. Often this means hiring new billing/finance/IT staff to track claims, denials, appeals, different billing systems, EHR integration, etc., rather than adding clinical or support staff. Further, the reimbursement rate is likely to be too low to cover all operating expenses, meaning supplemental fundraising is still an ongoing need. Check out the brief for more on both the pros and cons. (Tips: See our principles for reimbursement and consider partnering a medical respite program with a health center).
Hence, while a grants-based program has both advantages (more flexibility) and disadvantages (short-term funding), Medicaid reimbursement may reverse these — offering greater long-term sustainability but likely with less flexibility. So, yes, while Medicaid coverage is an important policy goal to pursue (and let’s keep pursuing it!), it’s important to prepare for the realities of working with insurance plans.
Final thought: It’s easy to get caught up in the financing details, but the ultimate goal is to meet the significant health care needs of unhoused people requiring recuperative care. Adding medical respite care into state Medicaid plans gives more tools for financing programs, aligns programs with the broader health care system, and improves quality of care.
More resources: The Council’s National Institute for Medical Respite Care (NIMRC) has numerous resources, including tool kits, program standards, issue briefs, a program directory, and other materials to increase the number of programs and ensure high quality care.
*“Medical respite care” and “recuperative care” are interchangeable terms.



