
Medicaid requirements and flexibilities during the COVID-19 public health emergency have protected the most vulnerable populations in our country. Lack of medical treatment is often a cause of homelessness, and continued barriers to care perpetuate suffering and poverty.
Medicaid opens the door for our patients to receive wraparound care for physical and social determinants of health. In conjunction with preventative and chronic disease care, Medicaid beneficiaries gain access to targeted case management that can assist with housing and social services navigation.
Medicaid provided an additional 17.7 million people with health insurance during the public health emergency; an increase of almost 25%. During the PHE, states were required to adopt continuous enrollment which prevented churn, or the frequent periods of disenrollment and re-enrollment, and in return received a 6.2% increase in the Federal Medicaid Assistance Percentage (FMAP). This has meant enrollees have not had to worry about losing coverage for the duration of the PHE; however, when it ends (currently set for January 15, 2023), the continuous enrollment provisions end.
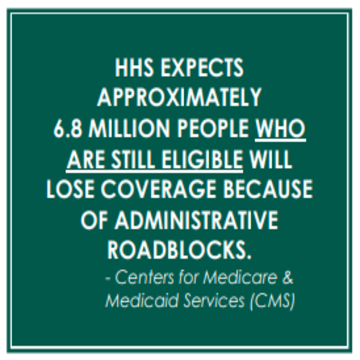
The Centers for Medicare and Medicaid Services (CMS) have identified some grim statistics. States will begin redetermining eligibility for Medicaid enrollees 60 days prior to the end of the PHE and people who are ineligible will lose insurance the last day of the month the PHE ends. If the PHE ends on January 15, 2023, the end date for continuous enrollment will be January 31, 2023. CMS projects that 9.5% of enrollees will lose coverage due to being ineligible, and an additional 6.8 million (or 7.9%) of Medicaid enrollees will lose coverage as a result of administrative churning even though they remain eligible. These patients may not have received their application due to an incorrect address, or may not have returned their forms on time.
People experiencing homelessness are disproportionately affected by administrative churn as they often have no reliable address where they can receive mail. To minimize this impact, enrollees should act now to update their contact information and health centers should learn their state’s process to complete redetermination on enrollees.
CMS, looking ahead to this possibly catastrophic and needless loss of coverage, has issued a proposed rule that should improve the redetermination process. The rule seeks to reduce administration burden by requiring electronic verification of income and assets for enrollees. States must make every effort to find the correct addresses for consumers before terminating coverage by searching their own databases, such as social services agencies and reliable third-party providers including managed care organizations. Under the proposed rule, redeterminations could not occur more than once a year, which will reduce the level of administrative churn. Implementing this rule will protect our consumers.

NEW COUNCIL RESOURCE
Medicaid redeterminations will likely occur beginning in January 2023, with disenrollments likely beginning in February. Our fact sheet describes how the HCH Community should prepare for Medicaid redeterminations as part of the public health emergency unwinding.
If you have questions please contact us on the Policy Team.
Let us know what you think.
